Dr. Koumanis has many years of experience in dealing with malignant skin cancers. The goal is for complete eradication of the skin cancer as well as a successful reconstruction. The ultimate goal also includes a good cosmetic outcome. Some growths turn out to be benign. Dr. Koumanis can also help in determining whether a skin growth is benign or malignant.
Dr. Koumanis covers patients from Warren, Saratoga, Washington, Albany counties and surrounding areas.
What is the recommendation for skin cancer screening?
There is no official recommendation for screening with regards to technique or time interval. That being said patients who are concerned with any strange looking growth should see their dermatologist, plastic surgeon or primary care physician as soon as possible.
Anyone with a previous history of skin cancer should be seen more often and this should be discussed with your physician or surgeon.
Skin Cancer Prevention
- Sun Avoidance– although some sun is good for vitamin D, overall health and feeling of well-being, the mid-day sun is the strongest and poses the most risk. This occurs between the hours of 10 am and 4 pm. Cloudy days still pose a threat as people are still exposed to harmful UVA/UVB rays.
- Sunscreen– applying sunscreen when out in the sun is a wise choice. It is recommended that application of sunscreen to exposed skin be SPF 30 or greater in strength. You must remember to reapply if sweating or going in and out of water.
- Avoid Tanning Beds– chronic use of tanning beds exposes you to harmful UV rays and can increase your chance of skin cancer.
- Cover Up– protective clothing that does not allow sun rays to penetrate, baseball caps, sunglasses and wide brimmed hats all help in reducing exposure to harmful sun rays. One can also buy SPF-material clothing and swimsuits.
- Self-Examination-look at your skin regularly and become familiar with any moles, freckles or blemishes. If anything looks concerning, please contact our office for an examination immediately.
- Screening– although there is no real recommendation for screening, skin cancers are very common and therefore if concerned about any area, please call us for an appointment. If your skin has numerous moles, freckles, growths or a strong family history of skin cancers exists then a full body screening may be in order.
What are the signs of skin cancer?
We look for the ABCDE signs of skin cancer. “A” stands for asymmetry of the lesion, “B” stands for border irregularity, “C” stands for nonuniform color, “D” stands for a diameter of greater than 6 mm and “E” stands for evolvement. That is the skin growth has noticeably been changing.
What are the different kinds of malignant skin cancer?
Theses are common enough that we see it in our practice with regularity. Merkel Cell Cancer is one that we see the least.
Basal Cell Cancer
Squamous Cell Cancer
Melanoma
Merkel Cell Cancer
What are the different kinds of benign skin growths?
Most skin growths or lesions are benign. Dr. Koumanis can examine you and sometimes by gross inspection can make the diagnosis. If there is any doubt about the skin growth a small biopsy can be obtained with minimal to no discomfort to the patient.
Benign Growths include:
Keratocanthoma
Seborrheic keratoses
Pyogenic Granuloma
Moles or Nevi
Dermatofibroma
Epidermal Inclusion Cyst
Lipoma
Some of the above are also soft tissue growths occurring in the deeper layers of the skin or subcutaneous tissues such as a lipoma or dermatofibroma. Benign growths are excised surgically if they bleed frequently, have grown large and cause obstruction or deformities.
Basal Cell Cancer
What is Basal Cell Cancer?
Basal cell cancer is a malignant skin cancer that originates from basal cells which are new skin cells formed as old ones die off. The DNA of that area of skin has mutated and caused the cells in the basal area to divide abnormally, causing basal cell cancer.
Although it is malignant this type of skin cancer is not fatal. Basal cell cancer is highly unlikely to metastasize to other parts of your body but in some instances can extend into muscle cartilage and bone of nearby structures if left untreated.
What are the signs and symptoms of Basal Cell Cancer?
Can range in color from a scaly clear lesion, to a red to brown color.
Can be crusty
Can sometimes grow bigger than digress but not go away
Can bleed especially on the face
These can occur in the face (most common), scalp, arms legs or body
What are the risk factors and causes of basal cell cancer?
Chronic sun exposure or ultraviolet light-repeated or prolonged exposure increases your chance of basal cell cancer
Living in high altitude areas increases your exposure to ultraviolet rays and thus basal cell cancer
Family or personal history-if you have had it before than recurrence or new basal cell cancer is more likely. Also, if it runs in the family you may be at increased risk of acquiring basal cell cancer.
Fair skin- light colored skin, hair and eyes leaves a person at increased risk of developing any malignant skin cancer including basal cell cancer.
Sex-males are at higher risk of developing basal cancer compared to woman.
Age-older individuals (i.e. greater than 50 years old) are at greater risk
Radiation- previous sites of skin exposed to radiation therapy may be at increased risk
Immune-suppressing drugs-persons who take these drugs are at increase the risk of developing skin cancers
Genetic Predisposition- certain inherited disorders such as Gorlin syndrome now known as “Nevoid Basal Cell Carcinoma Syndrome” and Xeroderma Pigmentosum are both associated with an abnormally high risk of basal cell cancer.
How do you diagnose Basal Cell Cancer?
Sometimes basal cell cancer growths can be diagnosed by examination alone. However, you may need a small biopsy to confirm the diagnosis before committing to treatment. This biopsy is done by numbing the area and then taking a small piece of the growth to send to a pathologist to confirm the diagnosis. This is quick, and patients experience minimal discomfort.
How is Basal Cell Cancer treated?
Topical Creams- ointments such as Effudex (fluorouracil), Aldara (imiquimod) and others are used for basal cell cancers that are less aggressive or more superficial. The patient applies the ointment for several weeks.
Surgery- the basal cell cancer is excised and then closed. If it is large, a flap or skin graft reconstruction may be needed. The margins of the specimen taken are examined under a microscope by a Pathologist to make certain that they are clear of the cancer cells.
Electrodessication and curettage- the basal cancer is scraped from the skin after numbing the area and then an electrocautery device attempts to destroy any remaining cells. The base can also be treated with cold liquid nitrogen to destroy the cells.
Mohs Surgery/Frozen Sections- in this method, the surgeon removes the basal cell cancer and then the specimen is excised in layers in three dimensions in order to make sure that all the margins are clear.
What are the possible complications?
Some of the complications include infection, bleeding, scarring, recurrence etc. The treatment involved with treating basal cancer is usually associated with minimal complication rates but Dr. Koumanis will discuss this along with treatment options at your consultation.
Squamous Cell Cancer (SCC)
Squamous cell cancer is the second most common skin cancer diagnosed in the United States. It is an abnormal growth of skin cells at the level of the epidermis (i.e. The most superficial layers of the skin or dermis)
It can occur on the skin anywhere on the body, and is very commonly found n the scalp, face and neck. In the face, nose, lips, ears and cheeks are very frequently the most common sites where one finds SCC. Note that SCC also occurs in deep organs and mucous membranes of the body but here we are discussing cutaneous or skin SCC. Squamous cell carcinoma can cause disfigurement and sometimes even death if not treated appropriately. Dr. Koumanis has many years of experience in treating SCC so you will be in good hands during your consultation.
What are the causes SCC and what are the risk factors?
The main causes are the same as Basal Cell Cancer such as UV radiation exposure from the sun or tanning beds. Risk factors include fair skin, HPV or human papilloma virus infection or exposure and certain precursor skin growths such as Aktinic or Solar Keratosis.
Aktinic/Solar Keratosis-scaly and crusty lesions or growths found on the skin after repeated sun exposure over many years usually. Aktinic Keratosis is considered a precancerous lesion because if left alone it can turn into Squamous cell cancer of the skin. The areas affected can become red or inflamed and can bleed sometimes due to friability.
Bowens Disease- this is considered an early stage of SCC. It is associated with the HPV, human papilloma virus and can sometimes be found on the genitals due to sexual transmission of the HPV. It can also be caused by repeated trauma or radiation exposure to the skin.
What is the treatment of squamous cell cancer?
Treatment options of Squamous Cell Cancer are similar to Basal Cell Cancer:
Surgical Excision
Mohs Surgery
Electrodesiccation and Curretage
Cryosurgery
Laser Surgery
Radiation Therapy
Melanoma
What is Melanoma?
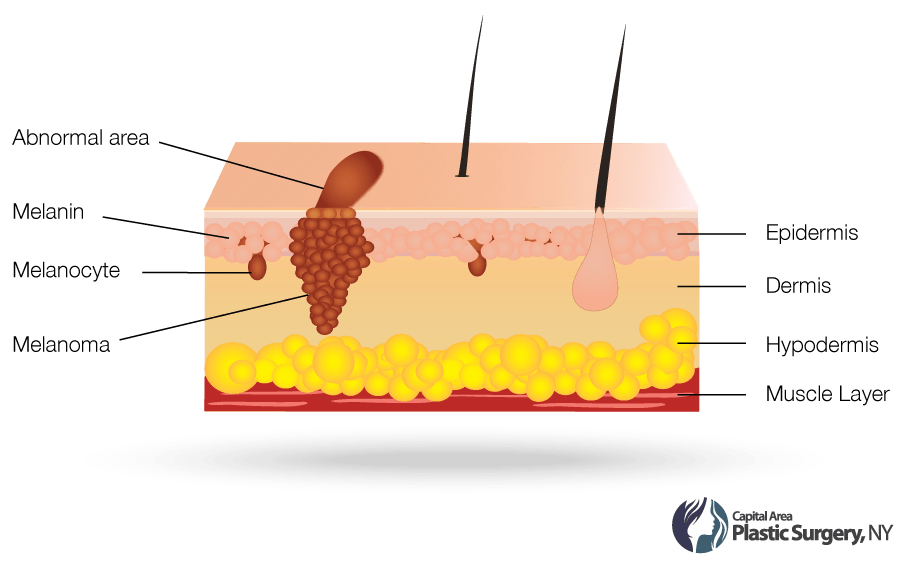
Melanoma is the most serious form of skin cancer and needs to be treated quickly and early. It occurs in the basal layer of the epidermis where the melanocytes live. Melanocytes are the cells that are responsible for pigmentation of the skin, especially during tanning. Melanoma occurs when the DNA structure of those cells have been disrupted or have mutated causing rapid multiplication of these mutated cells. Melanoma is a skin cancer that can metastasize to other parts of the body.
What are the causes and risk factors of Melanoma?
Sun/UV Radiation-sunburns and uv radiation increase the chance of melanoma. Early childhood sunburns with blistering leave one at risk later on in adulthood. People who live in places like Florida, California, Hawaii Australia etc. where more sunlight and UV radiation exposure occurs are at higher risk for developing Melanoma. Tanning bed use is also a risk.
Dysplastic Nevi-atypical or dysplastic moles are ones that have already started to change and are thought of as possible precursors to melanoma. These can occur sporadically or as part of an inherited syndrome.
Family History/Syndrome- if a parent or sibling has been diagnosed with melanoma than there is increased risk for occurrence due to hereditary links to the disease. Also, there is a syndrome called FAMMM which stands for Familial Atypical Multiple Mole Melanoma Syndrome. This is an inherited condition characterized by multiple atypical or dysplastic moles and a first or second degree relative with a history of melanoma.
Impaired Immune System- an immune system that is affected by organ transplant medications, HIV/AIDS or cancers such as lymphoma and leukemia increase the chance of melanoma.
What are the signs and symptoms of melanoma?
The ABCDE of melanoma is important to understand to catch it early or prevent it. Most moles are benign but if a patient has an overabundance of moles or freckles, has a strong family history then regular screening may be required. Each patient however should become familiar with their skin,
A- Asymmetry-the mole of growth will be asymmetrical in shape
B- Borders-the growth will show irregular borders and outlines whereas a healthy mole is smooth in shape.
C- Color-benign moles have a uniform color to them whereas melanoma is associated with several colors within its borders from brown, to purple and black.
D- Diameter-melanomas are usually larger than 6mm and benign moles are usually smaller however small melanomas occur early on as well.
E- Evolving-benign moles usually stay stable in appearance over time whereas a melanoma growth will change or evolve over time. Sometimes quickly as well.
Are there different types of melanoma?
There are many types of melanoma or variations of this disease. Some are more aggressive than others, but all are serious.
Superficial Spreading
Acral Lentiginous
Lentigo Maligna
Nodular
What is the treatment of Melanoma?
Surgical Excision -excision of the melanoma with wide enough margins is essential for eradication of the disease. The width of the margin chosen by the surgeon is based on the depth of the melanoma. Depths between 1mm and 4mm requires a sentinel lymph node dissection in the area of the melanoma and its corresponding draining patters. For example, a melanoma excised in the upper extremity would require an axillary lymph node dissection (i.e. arm pit)
The sentinel lymph node is the first lymph node that drains the area. Therefore, if that lymph node is clear then all others down stream by definition would be clear. If the sentinel node is positive with disease, then a full lymph node dissection is carried out usually. Mohs excision can also be performed for melanoma in recent years and is an option in some cases.
Immunotherapy-this is used for advanced melanoma with increased depth and/or metastases. It consists of immune system proteins used to fight off the cancer cells.
Chemotherapy-as immunotherapies have become preferable in treating advanced melanoma, chemotherapy has become second-hand in treatment.
Radiation Therapy-although radiation therapy is not considered first line treatment, it is sometimes used to control local recurrence in the area of a deep or advanced melanoma or to control lymph node spread. Radiation therapy is considered experimental rather than mainstay treatment.
How is the excision defect reconstructed?
After surgical excision or Mohs excision, a defect is left in the skin and subcutaneous tissue. If the defect is not wide, then a multilayered suture closure can be carried out. If the defect is large, then Dr. Koumanis will use numerous local flaps or skin grafting to close and reconstruct the area.
Merkel Cell Cancer
Merkel Cell Cancer is a very rare but ultra-aggressive skin cancer. It has a propensity for recurrence and metastases. It is caused by UV radiation and sun exposure just like melanoma.
What are the causes of Merkel Cell Cancer?
It is caused by UV radiation and sun exposure and occurs at a higher frequency in individuals with a compromised immune system. This incudes people with organ transplants, HIV/AIDS etc. Patients with lymphoma or leukemia histories and other autoimmune diseases have a higher chance of Merkel Cell Cancer.
What is the diagnosis and treatment of Merkel Cell Cancer?
The diagnosis is made with a skin biopsy and the treatments are very similar to Melanoma. Merkel Cell surgical excision requires a wide margin of excision, greater than that needed for melanoma usually. This is due to its aggressive nature.
REQUEST A CONSULTATION


